Abstract
Background: Sex chromosome loss (SCL) has long been deemed a physiological age-related phenomenon, but due to its increasingly common appearance in pathogenic settings, there has been renewed debate as to its clinical significance. In hematologic patients receiving sex-mismatched bone marrow transplantations (BMT), depending on the donor/patient sex combination, the appearance and/or disappearance of the Y chromosome can have various implications such as engraftment, relapse, or even donor cell leukemia. This diversity, especially when coupled with deletion/duplication of an X chromosome, can be extremely misleading when determining post-BMT chimerism and may even cause misdiagnosis. We investigated the incidence and clinical implications of SCL in patients who received sex-mismatched BMT.
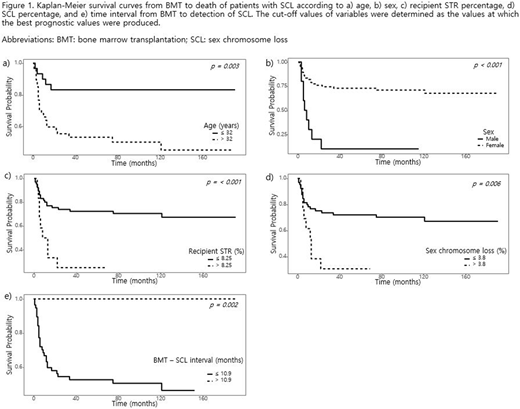
Methods: The present study includes 476 patients (262 females and 214 males) that underwent sex-mismatched BMT over a 10-year period (2005-2015) at Seoul National University Hospital. Retrospective review of electronic medical records was performed to obtain relevant clinical data. SCL was determined by X/Y Fluoresence in situ Hybridization (FISH) and its clinical significance was evaluated in conjunction with other available cytogenetic (karyotyping, FISH), molecular (short-tandem repeat (STR) analysis), and bone marrow (BM) aspiration/biopsy results. Correlation between clinical factors were analyzed via Kendall's rank correlation coefficients. Kaplan-Meier survival analysis was utilized to obtain and compare survival curves of the patients according to age, sex, recipient STR percentage, SCL percentage, and post-BMT time interval till appearance of SCL. Two types of survival was analyzed: the first being the survival from initiation of BMT, and the second being the survival from the onset of SCL.
Results: From a total of 476 patients who received sex-mismatched BMT, 77 patients (16.2%) showed post-BMT SCL. Interestingly, the number of female recipients with SCL was significantly higher than males (67 vs 10), but the overall degree of SCL (%) was higher in male patients. Acute myeloid leukemia (AML) was the most common primary diagnoses in all patients, but the distribution of diagnoses was not different between sexes. Females had a lower average age compared to males (33.8 vs 50.9 years). Correlation analysis showed that SCL positively correlated with both STR and age, however, there were a few cases with discrepancies between the SCL percentage and recipient STR percentage. These discrepancies usually occurred at low SCL and STR percentages (<5%), and required clinical interpretation via co-reviews of other available cytogenetic and/or molecular results. According to Kaplan-Meier survival analysis, the mortality rates measured from both initiation of BMT and onset of SCL were all significantly higher in patients >32 years (p=0.003, Figure 1 a), males (p<0.001, Figure 1 b), recipient STR >8.25% (p<0.001, Figure 1 c), SCL >3.8% (p = 0.006, Figure 1 d), and time interval from BMT to onset of SCL ≤10.9 months (p = 0.002, Figure 1 e). Comprehensive analyses of X/Y FISH combined with aberrant FISH markers, G-banding, and BM blast counts confirmed both higher relapse and mortality rates in SCL patients.
Conclusions: Vigilance is required when interpreting X/Y FISH results, especially when relatively low percentages (<5%) of SCL is present. In ambiguous cases, it is recommended to co-review cytogenetic and molecular results. Furthermore, based on the positive correlation of SCL with relapse and poor survival, we propose that SCL could have significant prognostic implications, and patients with SCL could be classified as high-risk and more carefully monitored in the post-BMT setting.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal